Learning patience, doing slimming exercises, building goals, while working the small motor skills and hand-eye coordination to build confidence is part of the recovery process at RINJ Women Shelters. Out-patient care is offered at some locations.
- War Survivors suffer Post Traumatic Stress Disorder (PTSD).
- Post Traumatic Rape Syndrome (PTRS) is suffered by rape survivors.
- PTRS is a different illness than PTSD .
The RINJ Foundation medical practitioners have become very talented in identifying PTSD and PTRS.
The most stressful events we encounter that contribute to this form of mental illness include:
- Childhood Rape
- Gender-Based Violence
- Rape and Attempted Murder (many women, children and men escape a violent rapist who is trying to kill them after the rape crime to prevent there being a criminal case with a survivor/witness testifying against them)
- War
Post traumatic rape disorders are serious mental illness problems despite male society’s denial and minimization efforts.
These patients, although the nature of the illness is to be reclusive and not seek help, desperately need assistance to return to a normal life.
If they do not receive the appropriate care, or manage to sort through the issues by talking to a trusted friend and coping, they may not survive the illness. A very high percentage of rape survivors commit suicide.
Symptoms of PTSD
- The survivor may have experienced or confronted with an event that involved actual or threatened injury, or a threat to their physical integrity. i.e. rape.
- The survivor may show symptoms of intense fear, helplessness or horror.
- The survivor may experience distressing recollections of the event. i.e. flashbacks.
- The survivor persistently avoids things that remind them of the event (triggers).
- The survivor may show significant distress or impairment, either in their social, occupational or other areas of functioning.
- Persistent symptoms of difficulty falling or staying asleep; irritability or outbursts of anger; difficulty concentrating; hyper vigilance; exaggerated startle response.
- Symptoms that last at least one month draw our closest attention.
PTRS Symptoms
- Intense fear, helplessness, or horror.
- Repeated and distressing recollections of the event, including images, thoughts, or perceptions. Such incidents are often called “flashbacks”.
- Distressing and or frightening dreams about the event.
- Associating various words, happenings, or “triggers” to the actual event which then causes a “flashback”.
- Avoidance of anything that may “trigger” a flashback including the avoidance of talking about the attack itself.
- Denial.
- A feeling of numbness, detachment or “unrealness” about everything.
- A lack of emotion or inability to feel love or care about anything.
- Feelings of depression; real depression; and isolation.
- A change in sleep patterns.
- Lack of concentration.
- Avoidance of being touched, and shying away from loved ones. Sudden movements may startle.
- Lack of trust in anyone, even close family or partners.
- More irritable than usual. Outbursts of anger and crying. Mood swings.
- A feeling of low self esteem and confidence.
- A feeling of being dirty, or disgusting.
- Deep embarrassment or shame. Sometimes self blame.
- Bitterness and morbid hatred of the perpetrator, with a preoccupation of how to harm or humiliate them.
- Loss of appetite or a change in eating patterns.
We can tell you in all honesty that from the minute that a patient contacts us looking for help, their new happiness begins. That’s very true. Just knowing you have done something to start ‘fixing’ your darkest nightmares, is a happy relief.
What Can You Expect From A Treatment Program
To find out, you will need to start. :o)
We can tell you here that you will gradually meet others with the same issues and it will surprise you how similar the symptoms are.
So that’s group therapy.
We would like you to read this document. It’s primarily intended for ‘Combined Joint Task Force Operation Inherent Resolve’ veterans coming from Iraq. We have used this doctrine for treating our own clinic security providers and caregivers alike. The more you learn, the better you will feel.
You are not alone. RINJ-dealing-with-PTSD
More about symptoms and why: RINJ-ptrs-ptsd_gbv-war-stress_english
You are going to talk about what happened with people who have had similar experiences.
Cognitive therapy is helpful for some patients. That’s pretty much one-on-one with a medical practitioner or mental health counsellor.
You are going to become well and in fact, you will likely be light years ahead of where you would have been had this traumatic experience not occurred.
Surviving is a very instinctive thing. Our minds and bodies have built in maximum-effort attributes for achieving survival. And when you survive a significant crisis you are actually a better person for the experience with the right treatment.
So, you are not going to be just feeling better, you will be a lot better than ever.
The depths of PTSD and what it means: Every day is going to be a hard day. Ask for help at RINJ Women’s shelters where PTSD counseling and group programs are free. Sliming-down exercising is another part of the RINJ Women Shelters project, explains Dr. Nassima al Amouri of The RINJ Foundation.
Don’t be afraid to ask for help.
Anger management
Techniques to reduce levels of anger and irritability with others are important. Strategies that are commonly used include the following:
- Education to understand the nature and purpose of anger
- Methods of identifying early warning signs of stress and irritability
- Methods of identifying high risk situations and how to prepare for them
- Methods of realistically re-evaluating the situation, keeping it in perspective
- Strategies to reduce arousal and stay calm in difficult situations
- Effective communication methods (verbal and non-verbal)
- Differentiating assertive from aggressive behaviour
- Problem solving strategies to effectively deal with disagreements
- Distraction and removal techniques to avoid “flare-ups”
- Practice in imagined and real-life situations
Management of depression
People with PTSD or PTRS frequently develop symptoms of depression. Some strategies to reduce and manage depression are:
- Increasing positive, enjoyable events and scheduling these into daily living
- Resolving the underlying assumptions and beliefs about the self (e.g., “I’m a worthless failure”) or the world (e.g., “Nobody cares about me”) that can lead to feelings of sadness and depression
- Identifying patterns of depressive thoughts on a day-to-day basis,
- Realistically evaluating and challenging negative beliefs and thoughts, and
- Rational, realistic coping self-talk.
Medication self-management
Medication is frequently used to help manage severe PTSD symptoms (although, on its own, it will not change the underlying problems and should be combined with psychotherapy treatment). To minimize unintended difficulties associated with medication, the following strategies are frequently used:
- Education about the use and effect of the substance,
- Education about possible side-effects and activities or substances to avoid,
- Methods of keeping track of medication use,
- Discussing the effects and desire to change medication with your psychiatrist, and
- Methods of reducing and stopping medication intake.
Substance abuse. A serious health issue.
Many people with PTSD attempt to cope or “self-medicate” with excessive amounts of alcohol and inappropriate drug use (including prescribed drugs). Treatment for substance abuse:
- Decisions regarding total abstinence versus controlled use of the drug,
- Recording “danger” times and identifying patterns of use,
- Developing coping strategies for high risk times,
- Assertiveness training for when others are applying peer pressure,
- Planning and scheduling activities not associated with the substance, and
- Response prevention methods of resisting the ‘urge’.
Sleep disturbance
Many sufferers of PTSD/PTRS report disturbances of sleep.
Several strategies may be useful in addressing the difficulty of going to sleep, waking repeatedly throughout the night, or waking early in the morning. It is common for therapists to assist clients in developing a healthy sleep routine in line with the suggestions provided above. Other strategies, including medication, may be adopted when those are not proving effective.
Relationship difficulties
People who have been traumatized often lose track of whom and what they can trust in the world. This often has a major impact on relationships. To address the difficulties that can occur between couples and family members, PTSD/PTRS sufferers are frequently taken through a range of strategies to improve relationships.
Some of the methods used may include active listening (how to really listen to your partner or children), communication training (how to say effectively what you need and feel), and problem solving (how to solve everyday problems without fighting). Some of this may occur with the survivor alone and some with their partner.
Separate support and counselling for the partner is often beneficial. Sometimes family therapy is provided, where the whole family meets to address their issues, with the aim of developing a healthy environment for all.
Exposure therapy Confronting feared situations
- Anxiety frequently causes people to stay away from the frightening situation. It is quite normal for people to want to escape or avoid situations, thoughts, memories, or feelings that are painful or distressing. However, this is one of the major impediments to recovery.
- Avoidance and escape provide temporary relief the anxiety reduces. Unfortunately, the next time the person encounters that situation, he or she is likely to become anxious long before it is planned to occur.
- We call this “anticipatory anxiety.” The more the situation is avoided, the more the person continues to believe that it is dangerous. Further, even if the person does not avoid, the anxiety may continue to build once they are in the situation.
Children present a another dimension in PTSD/PTSR treatments. If only mankind could exclude children from its violence.
 Some children survivors benefit from learning self-defence to improve their confidence.
Some children survivors benefit from learning self-defence to improve their confidence.- The motivation of this desire for self-protection is exploited to increase the patient’s exercise which itself is part of the therapy.

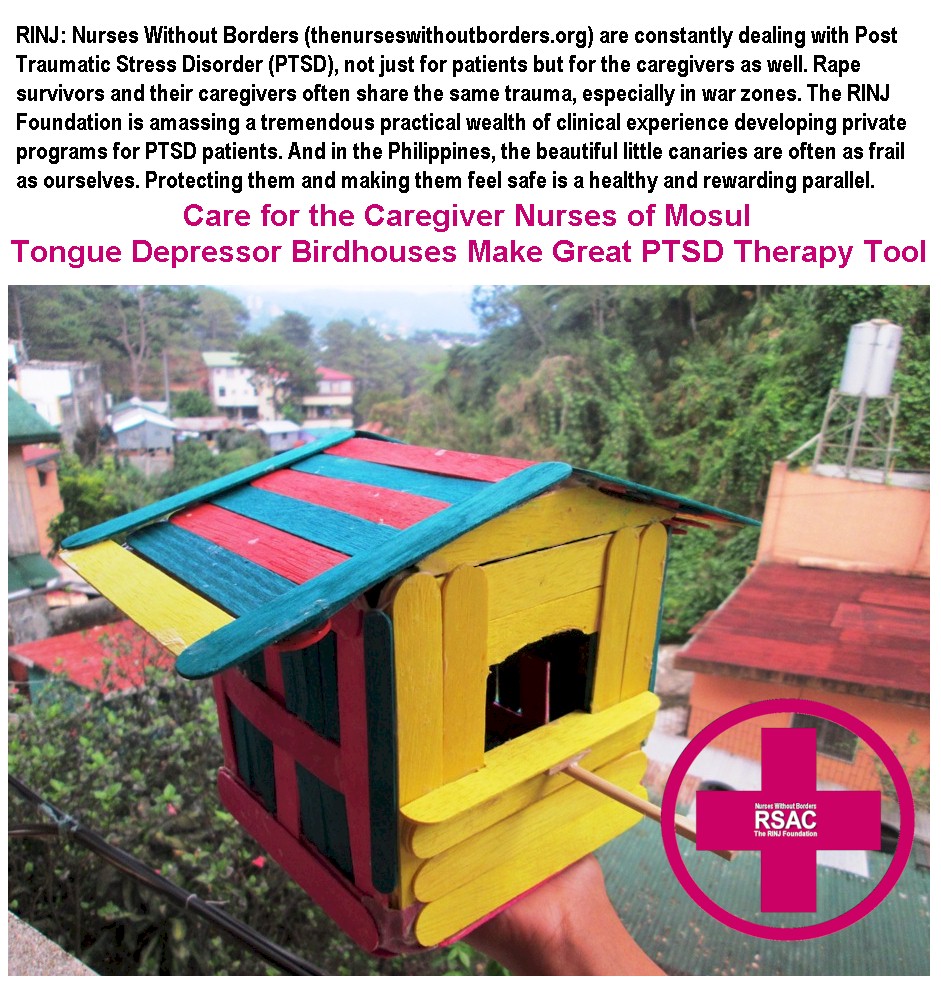
Learning patience while working the small motor skills and hand-eye coordination to build confidence.